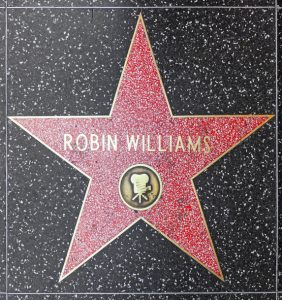
 On July 21, 2021, comedian and actor Robin Williams would have turned 70. Seven years prior, he suffered from an undiagnosed neurodegenerative disease, later determined to be Lewy Body Dementia, which led him to take his own life.
On July 21, 2021, comedian and actor Robin Williams would have turned 70. Seven years prior, he suffered from an undiagnosed neurodegenerative disease, later determined to be Lewy Body Dementia, which led him to take his own life.
Williams’ suicide brought awareness to the life-changing, fatal disease known as Lewy Body Dementia, and his passing brought much needed attention to the importance of mental health and symptoms of depression and anxiety that can accompany a neurodegenerative disease such as Parkinson’s.
What Do We Know About Lewy Body Dementia?
Nearly seven years after Robin Williams’ passing, what do we know about Lewy Body Dementia (LBD)? How can we help people with a neurological disease experiencing suicidal thoughts? A documentary made after Robin’s passing that delves deeper into his experience with the disease can possibly help answer these questions.
“Robin’s Wish,” a documentary released this past year, chronicles Robin Williams’ experiences with and symptoms of LBD. The film describes the disease, how it affected his personal and professional life, and current research efforts to understand and treat it. This documentary is the passion product of his wife, Susan Schneider Williams, to educate people about LBD, so that other families do not have to go through the heart-wrenching experiences that she and Robin endured.
Robin’s Final Year Is Documented in Film
In the last year of his life, at the age of 63, Robin Williams experienced a pattern of behavior that was unusual for him. He began displaying odd symptoms, including personality changes, confusion, forgetfulness, anxiety, paranoia, hallucinations, and problems with movement. Friends, family, and film colleagues recognized that he was not himself. They suspected that perhaps he was suffering from a severe psychiatric disorder such as depression or schizophrenia. He too felt that something was wrong, but he did not know what or why. Robin and Susan sought help from a variety of medical specialists, but there were no definitive answers. It was not until after his death that his autopsy showed that he had an extremely advanced case of LBD, with clumps of protein known as Lewy bodies found throughout his entire brain.
This diagnosis led Susan on a quest to raise awareness of the disease. LBD is a less well-known form of dementia that affects approximately one million Americans. There is considerable overlap between LBD and the cognitive decline that occurs in many individuals with long-standing Parkinson’s disease.
Since Robin’s death, Susan has immersed herself in becoming an advocate for LBD awareness and thus contributed to the production of “Robin’s Wish.” When the film was in production, Susan came to the National Institute of Health to interview lab chiefs and program directors. They discussed the distinction between neurological disorders, such as LBD, and severe psychiatric disorders. The scientists explained that they are all consequences of disorders of the brain’s circuitry. “When there is a miswiring in the brain for any reason, pathologic behavior or loss of cognitive abilities can result,” they said.
The theatrical release of “Robin’s Wish” started streaming this past fall on video on demand services. Scientists at the Lewy Body Dementia Association also produced a medical/scientific version of the documentary for the healthcare community. This second version of the film was featured at a launch party on October 29th.
What “Robin’s Wish” Teaches Us about Lewy Body Dementia
The first major film about a person with LBD, “Robin’s Wish” tells the story of what people with this devastating disorder are really struggling with. Explaining the movie’s title and Williams’ main “wish,” Schneider Williams said the Oscar winner “wanted to help all of us be less afraid.”
The film explains how LBD is a progressive brain disorder that is diagnosed when cognitive decline is an early symptom. It can also be diagnosed when cognitive decline and motor symptoms begin and develop together.
According to The Guardian, “When she (Susan Schneider Williams) first had the idea of making a movie about LBD, she pitched it as a straight science film (“the director laughed”). So she compromised and made “Robin’s Wish” a very affecting documentary about her husband’s experience of the illness. “If my husband weren’t famous I would not have put myself through this. But there were so many misunderstandings out there about what had happened to him, and about Lewy bodies. So this felt like the right thing to do,’” she says.
We learn from the film and other sources that “Lewy Body Dementia is a common type of dementia — it is the second most common neurodegenerative dementia behind Alzheimer’s,” said Jennifer G. Goldman, MD, MS, section chief of Parkinson’s Disease and Movement Disorders at Shirley Ryan AbilityLab and a professor in Physical Medicine and Rehabilitation and Neurology at Northwestern University Feinberg School of Medicine. “With greater education and awareness, with Lewy Body Dementia including both Dementia with Lewy Body and Parkinson’s disease (PD) dementia, we can start to change that landscape.”
What is the Difference Between Lewy Body Dementia and Parkinson’s Disease Dementia?
Lewy Body Dementia is a term used for both Parkinson’s disease dementia and Lewy Body Dementia. They have some things in common, but their progression and treatment are different.
While many people with Parkinson’s can experience cognitive changes, it is important to know that not everyone with Parkinson’s will develop dementia. With Parkinson’s dementia, the motor symptoms are present before the dementia. In Lewy Body Dementia, the initial core symptom is dementia — cognitive changes are early, and motor features, if present, occur either after the onset of dementia or concurrently.
Fight for a Diagnosis
Before Robin Williams was diagnosed with Lewy Body Dementia, it was reported that he had been experiencing paranoia, confusion, insomnia, constipation, and an inability to smell. For many, the wide range of early symptoms — not all related to brain function — makes Lewy Body Dementia difficult to diagnose.
Dr. Goldman urges patients to fight to find their diagnosis. “Continue to seek the answers and seek out a specialist to help identify the cause of the cognitive issues or type of dementia,” said Dr. Goldman. “The right doctor can change one’s management, prognosis, and eligibility for participating in research studies. It’s important to have the best understanding of the disease for the chance to have the best outcomes.”
LBD and Depression and Suicide
It’s also important to be aware that people with neurological conditions, such as LBD, are at higher risk for suicide, according to a study published in the Journal of the American Medical Association in February 2020. Depression can be a common symptom of LBD.
People living with LBD benefit most from a team-based health care approach that includes a mental health professional. With a team in place, should depression or suicidal thoughts occur, you have an established relationship with a professional you trust. However, it is never too late to add a mental health professional to your care team.
If you or your loved one is having thoughts of suicide:
- Find the resource that works for you: Twenty-four-hour suicide prevention hotlines can help, such as the National Suicide Prevention Lifeline at 1-800-273-8255.
- Seek professional help: Find a psychologist, therapist, counselor, or social worker you can trust and lean on.
- Stay engaged: It can be easy for people with Parkinson’s to distance themselves. Try to connect with family and friends, schedule regular phone calls, seek out a support group or wellness class.
- If you are a care partner or family member, learn about suicide warning signs and how you can help here.
Get Diagnosed Early and Take Advantage of Treatment Options for LBD
There are treatment options for LBD. Health care teams are finding that the most effective approach is a combination of medication, physical and mental exercises, and incorporating a mental health professional as part of a care team.
Robin Williams brought so much joy to so many people through his acting and his charity work, and there is no doubt that he will always be cherished for his brilliant performances on screen and stage. “Robin’s Wish” honors his wish of helping other people “to be fearless.” We hope that his film and other LBD awareness efforts can play a supporting role in making this wish come true.
Think You or a Loved One Have LBD or Another Form of Dementia?
Doctors can accurately diagnose symptoms of dementia in 90 percent of cases. If you know someone who appears to be losing mental abilities to a degree that interferes with daily activities and social interactions, consult a doctor right away. There are some medications and treatments that may help manage some of the symptoms, so it’s important to seek help as soon as possible.
Persons with LBD and other forms of dementia and their families face special legal and financial needs. Controlling the high costs of caring for a loved one with LBD, and navigating the emotionally and physically demanding requirements of care giving require the assistance of a highly skilled and specialized expert in the field of elder law.
For an initial consultation:
Fairfax Lewy Body Dementia Planning: 703-691-1888
Fredericksburg Lewy Body Dementia Planning: 540-479-1435
Rockville Lewy Body Dementia Planning: 301-519-8041
DC Lewy Body Dementia Planning: 202-587-2797














Leave a comment
You must be logged in to post a comment.